We have compiled the information regarding pregnancy, breastfeeding and corona virus from different reliable sources including WHO. The sources are mention at the end of the article, the information is just for educational purpose and do not offer an alternative to a doctor’s advice.
How Corona virus Affect Pregnancy and postpartum
1. Risk of COVID-19 during pregnancy
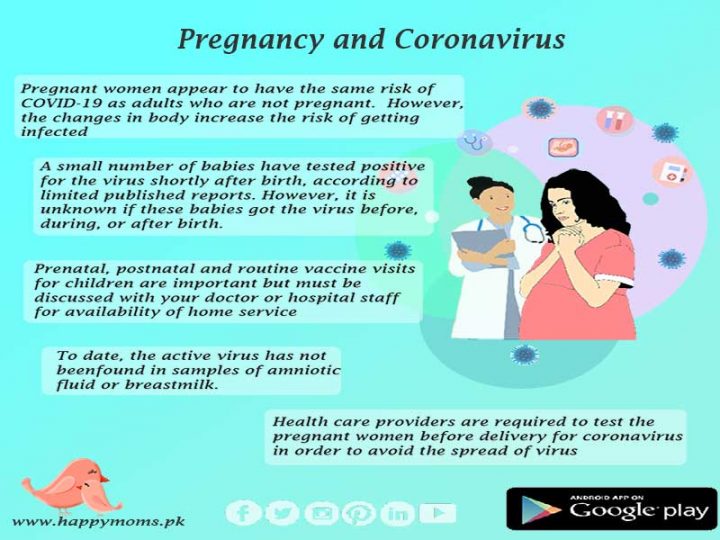
Pregnant people appear to have the same risk of COVID-19 as adults who are not pregnant. However, much remains unknown. We do know that pregnant people have had a higher risk of severe illness when infected with viruses that are similar to COVID-19, as well as other viral respiratory infections, such as influenza.
We also know that pregnant people have changes in their bodies that may increase their risk of some infections. Therefore, if you are pregnant, it is always important for you to try to protect yourself from illnesses whenever possible.
Risks to the baby
- Much is still unknown about the risks of COVID-19 to the pregnancy and to the baby.
- Mother-to-child transmission of COVID-19 during pregnancy is unlikely. However, after birth, a newborn can be infected after being in close contact with an infected person, including the baby’s mother or other caregivers.
- Emerging evidence suggests that transmission from a woman to her baby during pregnancy or birth (vertical transmission) is probable. It is important to emphasize that in all reported cases of newborn babies developing coronavirus very soon after birth, the babies were well.
- A small number of babies have tested positive for the virus shortly after birth, according to limited published reports. However, it is unknown if these babies got the virus before, during, or after birth.
- A small number of other problems, such as preterm birth, have been reported in babies born to mothers who tested positive for COVID-19 late in their pregnancy. However, we do not know if these problems were related to the virus.
- To date, the active virus has not been found in samples of amniotic fluid or breastmilk.
2. Prenatal and postpartum care during the COVID-19 pandemic
Should I attend my postnatal and antenatal appointments?
It is important to take care of yourself and your baby during pregnancy and after delivery. Your antenatal and postnatal appointments remain an important part of your maternity care to provide checks and screening on your health and your baby’s health.
Do not skip your prenatal care appointments or postpartum appointments. If you are concerned about attending your appointment due to COVID-19, talk to your doctor or hospital representative.
- Ask your doctor about how they are taking steps to separate healthy patients from those who may be sick.
- Some healthcare providers might choose to cancel or postpone some visits. Others may switch certain appointments to telemedicine visits, which are appointments over the phone or video. These decisions will be based on the circumstances in your community as well as your individual care plan.
- Do not delay getting emergency care because of COVID-19.
- You should continue to contact your doctor by telephone to discuss any questions or concerns you might have and to check on arrangements for all scheduled and future appointments.
Will my baby be tested for CORONA VIRUS?
If you have confirmed or suspected coronavirus when the baby is born, doctors who specialize in the care of newborn babies (neonatal doctors) will examine your baby and advise you about their care, including whether they need testing.
Well visits and routine vaccine visits for children
Newborn visits. Ideally, newborn visits should be done in person so that your pediatric healthcare provider can check your baby’s growth and feeding, check your baby for jaundice, make sure your baby’s newborn screening tests were done, and get any repeat or follow-up testing, if necessary. At the newborn visit, your pediatric healthcare provider will also check how you and your baby are doing overall. Newborn screening tests include a bloodspot, hearing test, and test for critical congenital heart defects..
- Vaccine visits. Vaccines are an important part of keeping your child healthy, especially if your child is under 2 years old. Vaccines help provide immunity before being exposed to potentially life-threatening diseases. Although there is not yet a vaccine to help protect against COVID-19, vaccines for illnesses such as measles, influenza (flu), whooping cough (pertussis), and other infectious diseases are important for your child’s health. This will help to prevent outbreaks of vaccine-preventable diseases among young children during the COVID-19 pandemic.
- Ask your healthcare provider how they are taking steps to separate healthy patients from those who may be sick. Some health care providers may choose to delay visits like well child checks and routine vaccine visits. These decisions will be based on circumstances in your community and your child’s individual care plan. Call your hospital or government center to ask about any upcoming appointments or about when your child’s vaccinations are due.
- Check for center which provide home services in your city.
3. Selecting Delivery locations during the COVID-19 pandemic
Delivering your baby is always safest under the supervision of trained healthcare professionals. If you have questions about the best place to deliver your baby, discuss them with your gynecologist beforehand.
In Pakistan many hospitals have stopped taking delivery cases, some doctors are not practicing during this time. Yet there are many hospitals providing the services to gynae patients, it is better to discuss all your concerns with your doctor beforehand and get details of the hospital you are choosing to deliver.
How will I be tested for CORONAVIRUS?
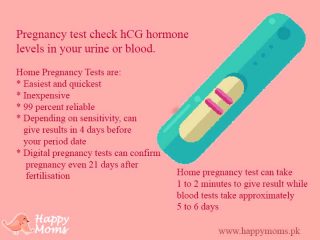
The process for diagnosing corona virus infection is changing rapidly. Testing is now open to anyone, including pregnant women, with corona virus symptoms. You should visit the government designated hospitals and centers for getting your test done
To minimize the spread of corona virus in hospitals, the offer of testing is being expanded to include all patients admitted to hospital, regardless of whether they have coronavirus symptoms or not. This includes offering tests to all women who attend hospitals for urgent or emergency maternity care, including attendance for spontaneous labour and birth.
Pregnant women are tested in the same way as anyone else. Currently, the test involves swabs being taken from your mouth and nose. You may also be asked to cough up sputum, which is a mixture of saliva and mucus.
The most effective tests currently take 24–48 hours for the result to be available
What is an antibody test?
You may also have heard about antibody testing for coronavirus. This is a blood test that can show whether you have previously come into contact with the virus or not. It does this by detecting antibodies, which your body produces if you have had coronavirus. This is called an immune response.
4. What is my risk of becoming very ill if I do have COVID-19?
Given that this is a novel virus, little is known about its impact on pregnant women. At this time:
No evidence shows that being pregnant increases a woman’s risk for getting COVID-19, or her risk of developing severe symptoms if she has the disease.
Experts think that pregnant women are just as likely as the general public to develop symptoms if infected with the new coronavirus. Current information suggests symptoms are likely to be mild to moderate, as is true for women (and men) in this age range who are not pregnant.
Does becoming ill with COVID-19 increase risk of miscarriage or other complications?
An increased risk of miscarriage or fetal malformations has not been documented in pregnant women who are infected with COVID-19, according to the CDC. Based on data from other coronaviruses, such as SARS and MERS, the American College of Obstetricians and Gynecologists notes that pregnant women who get COVID-19 may have a higher risk for some complications, such as preterm birth. However, this data is extremely limited, and the infection may not be the direct cause of preterm birth.
5. Self-Isolation
What should I do if I think I may have coronavirus or been exposed?
If you are pregnant and you have either:
- a high temperature or
- a new, continuous cough or
- a loss or change to your sense of smell or taste
you should stay at home for 7 days. Do not go to a GP surgery, pharmacy or hospital without contacting them on the telephone first
What should I do if I test positive for coronavirus?
If you test positive for coronavirus outside of a hospital setting, you should contact your doctor or hospital team to make them aware of your diagnosis. If you have no symptoms or mild symptoms, you will be advised to recover at home. If you have more severe symptoms, you might be treated in hospital.
Why would I be asked to self-isolate?
You may be advised to self-isolate because:
- You have symptoms of coronavirus, such as a high temperature or new, continuous cough, or loss or change in your sense of smell or taste
- You have tested positive for coronavirus and you’ve been advised to recover at home
- You have an elective caesarean birth or induction of labour planned and you have been asked to self-isolate prior to your admission to hospital
Can I still go to antenatal appointments if I am self-isolating?
You should contact your doctor/hospital to inform them that you are currently in self-isolation for possible/confirmed coronavirus and ask for advice on going to routine antenatal appointments.
What happens if I go into labour during my self-isolation period?
- If you go into labour during self-isolation, you should call your maternity unit for advice, and inform them that you have suspected or confirmed coronavirus infection.
- If you have mild symptoms, you will be encouraged to remain at home (self-isolating) in early labour, as usual practice.
- Your maternity team have been advised on ways to ensure that you and your baby receive safe, quality care, respecting your birth choices as closely as possible.
6. COVID-19 and children
There is much more to be learned about how this disease affects children. While some children and infants have been sick with COVID-19, most illnesses have been among adults. Some reports suggest that infants under 1 year old and those with underlying medical conditions might be at higher risk of serious illness from COVID-19 than other children.
- Children with COVID-19 generally have mild, cold-like symptoms, such as fever, runny nose, and cough. Vomiting and diarrhea have also been reported in some children.
- Children with certain underlying medical conditions, such as chronic lung disease or moderate to severe asthma, serious heart conditions, or weak immune systems, might be at higher risk for severe illness from COVID-19.
Face shields for newborns and infants
It is recommended that everyone 2 years and older wear a cloth face covering that covers their nose and mouth when they are out in the community. Because of the danger of suffocation, do NOT put cloth face coverings on babies or children younger than 2 years.
7. Breastfeeding and Coronavirus
Can I continue Breastfeeding if I have COVID-19
- Breast milk provides protection against many illnesses and is the best source of nutrition for most infants.
- You, along with your family and doctor, should decide whether and how to start or continue breastfeeding.
- We do not know for sure if mothers with COVID-19 can spread the virus to babies in their breast milk, but the limited data available suggest this is not likely. WHO recommends continuing breastfeeding even if mother is tested positive, with precautions
If you have COVID-19 and choose to breastfeed:
- Wear a cloth face covering while breastfeeding and wash your hands before each feeding.
If you have COVID-19 and choose to express breast milk:
- Use a dedicated breast pump.
- Wear a cloth face covering during expression and wash your hands before touching any pump or bottle parts and before expressing breast milk.
- Follow recommendations for proper pump cleaning after each use, cleaning all parts that come into contact with breast milk.
- If possible, expressed breast milk should be fed to the infant by a healthy caregiver who does not have COVID-19, is not at high-risk for severe illness from COVID-19, and is living in the same home.
The well-recognized benefits of breastfeeding and the protection it offers to babies outweigh any potential risks of transmission of coronavirus through breastmilk. Provided your baby is well and doesn’t require care in the neonatal unit, you will stay together after you have given birth so skin-to-skin and breastfeeding can be initiated and supported if you choose.
When you or anyone else feeds your baby, the following precautions are recommended:
- Wash your hands before touching your baby, breast pump or bottles
- Try to avoid coughing or sneezing on your baby while feeding at the breast
- Consider wearing a face mask while breastfeeding, if available
- Follow recommendations for pump cleaning after each use
- Consider asking someone who is well to feed your expressed breast milk to your baby.
If you choose to feed your baby with formula or expressed milk, it is recommend that you follow strict adherence to sterilization guidelines.
8. Managing stress during pandemic
How can I protect my mental WELL BEING during the pandemic?
Pandemics can be stressful for everyone. Fear and anxiety about a disease can be overwhelming and cause strong emotions in both adults and children. Coping successfully with stress will make you, the people you care about, and your community stronger.
Talk with your children about the pandemic. It is important to try to stay calm and to give children information that is truthful and appropriate for their ages and developmental levels. Children respond differently to stressful situations than adults.
- Depression during and after pregnancy is common and can be treated. Postpartum depression is depression that can happen after having a baby. If you think you may be experiencing depression, seek treatment from your health care provider as soon as possible.
- Pregnant people and parents caring for young children may be experiencing increased stress due to the COVID-19 pandemic.
The information shared is recommendations from sources available online and are given below. We do not take responsibility of your reliance on any information provided here.
Sources
Coronavirus infection and pregnancy, Royal College of Obstetricians and Gynecologists
COVID-19 : Resources for Pregnancy, Childbirth, Postnatal Care, WHO
Pregnant and worried about the new coronavirus?, Harvard Health Publishing
Experience shared by Mothers who delivered during Pandemic (Covid 19)


Thank you for this